The perineum is the region located between the genital area and the anus and plays a vital role in essential bodily functions such as childbirth, urination, and bowel movements. Its purpose is to provide support to reproductive organs and pelvic floor muscles. Experiencing pain in this delicate region can significantly impact an individual’s overall quality of life and daily activities.
What Is Perineal Pain?
Defining perineal pain, the International Continence Society describes it as the sensation of pain occurring between the posterior fourchette (the posterior lip of the introitus) and the anus in females and between the scrotum and the anus in males1.

Before delving into the causes, symptoms and other aspects associated with perineal pain, we will discuss the coping mechanisms for this condition.
How To Ease Perineal Pain
While specific strategies may vary depending on the root cause of perineal pain, the following non-surgical and surgical options are some general coping mechanisms and management options for perineal pain:
A. Non-Surgical Interventions:

1. Medical Consultation:
Addressing perineal pain begins with promptly seeking medical attention to identify its underlying cause. A comprehensive assessment, including history-taking and examination by a healthcare professional, is crucial for an accurate diagnosis.
2. Pain Management Techniques:
Various strategies can help alleviate pain, including over-the-counter pain relievers, prescribed medications, or topical analgesics.
3. Warm Sitz Baths:
Soothing perineal discomfort is possible through warm sitz baths, particularly beneficial in cases of inflammation, muscle tension, or post-childbirth.
4. Pelvic Floor Physical Therapy:
Specialized physical therapy programs like Kegel’s exercise address musculoskeletal issues contributing to perineal pain, especially in conditions like pelvic floor dysfunction.
5. Lifestyle Modifications:
Implementing changes in daily habits, such as maintaining good posture, avoiding prolonged sitting, and incorporating regular physical activity, contributes to perineal pain management.
6. Topical Treatments:
The application of over-the-counter or prescribed topical creams, ointments, or suppositories provides relief for specific types of perineal discomfort, such as hemorrhoids or fissures.
7. Biofeedback:
Biofeedback therapy enhances awareness and control of pelvic floor muscles, aiding conditions like pudendal neuralgia or pelvic floor dysfunction.
8. Psychological Support:
Managing the emotional impact of perineal pain is crucial. Counselling, support groups, or mindfulness techniques help address stress and anxiety associated with chronic pain.
9. Perineal Massage:
Guided by a healthcare professional, perineal massage techniques can benefit conditions like scar tissue formation or improve tissue elasticity, alleviating perineal pain.
10. Hygiene Practices:
Maintaining good perineal hygiene, especially after bowel movements, prevents further irritation and promotes healing in individuals with perineal pain.
11. Nutrition:
A fibre-rich diet and adequate hydration help prevent constipation, reducing strain during bowel movements and alleviating perineal pain.
12. Supportive Devices:
In some cases, cushions or pillows may be recommended to relieve pressure on the perineal area, especially during prolonged sitting.
B. Surgical Interventions:

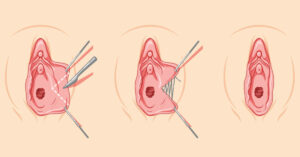
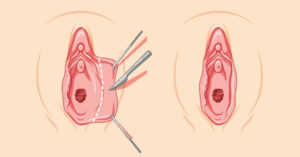
1. Perineoplasty
When conservative measures fall short, surgical interventions like perineoplasty (sometimes also called perineal scar revision) may be considered to address specific underlying issues. Individualizing the management approach based on the specific diagnosis and needs of the individual experiencing perineal pain is crucial.
What Causes Perineal Pain?

Perineal pain encompasses a range of potential causes:
1. Injuries and Trauma:
Childbirth-Related Trauma: Injuries resulting from childbirth, like perineal tears or episiotomies, can lead to discomfort or pain in the perineal region.
Accidental Trauma: Unintentional incidents such as falls or direct trauma can result in perineal pain.
2. Infections:
Formation of Perineal Abscess: The accumulation of pus within perineal tissues can be a contributing factor.
Sexually Transmitted Infections (STIs): Infections like herpes or gonorrhea can manifest with associated perineal discomfort or pain.
3. Inflammatory Conditions:
Pelvic Inflammatory Disease (PID): Inflammation affecting reproductive organs can extend to the perineum.
Inflammatory Bowel Disease (IBD): Conditions such as Crohn’s disease or ulcerative colitis may cause perineal pain.
4. Nerve-related Issues:
Pudendal Neuralgia: Chronic perineal pain may arise from compression or pudendal nerve irritation.
Neuropathy: Conditions causing nerve damage, such as diabetes, have been implicated in perineal pain.
5. Musculoskeletal Causes:
Pelvic Floor Dysfunction: Anomalies in pelvic floor muscle function can be a factor in pelvic and perineal pain.
Coccydynia: Pain in the coccyx or tailbone has the potential to radiate to the perineum.
6. Urological Issues:
Urinary Tract Infections (UTIs): Infections within the urinary tract can induce perineal pain.
Prostatitis: Inflammation of the prostate in males may contribute to discomfort in the perineal region.
7. Gynecological Conditions:
Endometriosis: The presence of endometrial tissue beyond the confines of the uterus can provoke perineal pain.
Ovarian Cysts: Enlarged cysts may induce discomfort, extending to the pelvic region, including the perineum.
8. Psychological Factors:
Pelvic Floor Tension Myalgia: Chronic pelvic pain characterized by muscular tension may be influenced by psychological factors such as stress or anxiety.
A thorough evaluation by a specialist is essential for an accurate diagnosis, leading to targeted and effective management. A multidisciplinary approach involving gynecologists, urologists, and pain management experts may be crucial for a holistic approach to care.
What Are The Symptoms of Perineal Pain?

Perineal pain manifests with various symptoms, showcasing the complex nature of this condition. Those experiencing perineal pain commonly report:
- Dull Aching or Persistent Discomfort: A prevalent manifestation involves persistent and dull aching sensations in the perineum.
- Burning or Tingling Sensations: Some individuals describe burning or tingling feelings, possibly indicating nerve involvement or inflammation in the perineal area.
- Sharp or Shooting Pain: Occasional sharp shooting pains may accompany specific movements or activities, such as sitting or bowel movements.
- Tenderness Upon Palpation: This is commonly detected during clinical examination, indicating localized sensitivity.
- Experiencing pain during sexual intercourse: Also known as dyspareunia, this is a notable symptom.
- Difficulties or discomfort during bowel movements.
- Urinary Symptomatology: Discomfort during urination, changes in urinary frequency, or urgency may coincide with perineal pain, indicating possible involvement of the urological domain.
- Visible Signs of Inflammation: Observable signs like swelling or redness in the perineal area may be seen.
- Pain radiating to adjacent areas like the lower abdomen, thighs, or lower back suggests potential involvement of nearby nerves or structures.
- Apart from physical symptoms, perineal pain can have an emotional impact, leading to anxiety, stress, or mood disturbances. Recognizing and addressing the psychological aspects of pain is crucial for a comprehensive approach.
Recognizing the various origins of perineal pain is crucial, and the varied symptom presentation helps narrow down potential diagnoses. This comprehensive blog post serves as a valuable resource for those seeking information on perineal pain, its causes, management strategies, and the potential role of perineoplasty in addressing specific conditions.
Choose The Right Surgeon For Your Perineoplasty
Perineoplasty is a specialized surgical procedure focused on reconstructing the perineum, often to repair damage or enhance comfort and aesthetic appearance. This surgery requires a skilled surgeon, as it involves precise techniques to ensure both functional and cosmetic improvements. The success of a perineoplasty significantly depends on careful preoperative planning, expert surgical execution, and diligent postoperative care to achieve the desired results safely and effectively.

Anyone considering this surgery should thoughtfully consider their options, consulting with experienced professionals. We recommend booking a no-commitment consultation with the specialists at Alinea Labiaplasty & Vaginoplasty Michigan to gain deeper insights into the procedure.
References
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29: 4–20, 2010.
- Homma Y. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee the International Continence Society. J. Jpn Neurogenic Bladder Soc.. 2003;14:278-89.
- Furnas HJ, Canales FL. Vaginoplasty and perineoplasty. Plastic and Reconstructive Surgery Global Open. 2017 Nov;5(11).